Introduction
What Autoimmune Disease Causes Hives? Hives, also known as urticaria, are itchy, raised welts on the skin that can appear suddenly and vary in size and shape. While hives are generally touched off by disinclinations, infections, stress, or environmental factors, they can also be caused by autoimmune conditions. Autoimmune conditions occur when the vulnerable system inaptly attacks the body’s cells and apkins, leading to habitual inflammation and colorful symptoms, including hives.

In this composition, we will explore the autoimmune conditions that can beget hives, their symptoms, opinions, and treatment options to help individuals manage their condition effectively.
Understanding Hives in Autoimmune Conditions
Hives occur when the vulnerable system releases histamine and other chemicals into the skin, causing swelling and greenishness. In autoimmune conditions, this vulnerable response can be patient, leading to habitual urticaria( hives lasting further than six weeks). Autoimmune urticaria is frequently linked to underpinning health conditions, where the body inaptly targets its cells, including the mast cells responsible for antipathetic responses.
What Are Hives?
Hives, also known as urticaria, are red, itchy welts that appear on the skin due to an immune system reaction. While they are often triggered by allergies, infections, or environmental factors, they can also result from autoimmune conditions. In these cases, the immune system mistakenly attacks the body’s tissues, leading to persistent or chronic hives. Unlike allergic reactions, which typically resolve quickly, autoimmune-related hives can last for weeks or months and may not respond well to standard antihistamine treatments.
Autoimmune Diseases That Cause Hives
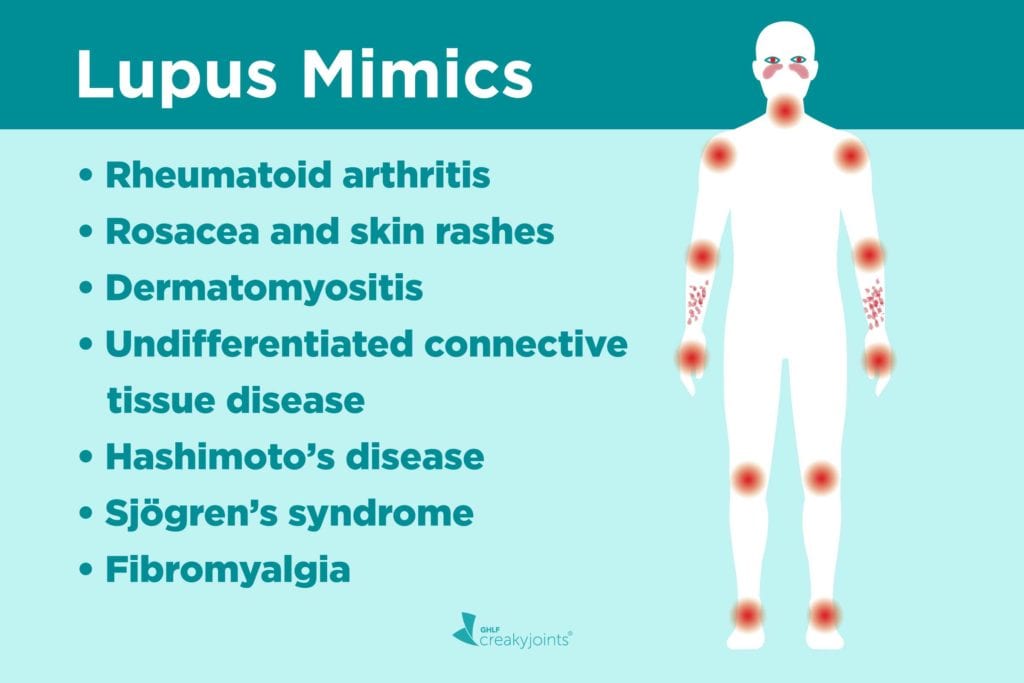
Several autoimmune diseases are associated with chronic hives, including lupus, rheumatoid arthritis, and thyroid disorders such as Hashimoto’s thyroiditis and Graves’ disease. In these conditions, the immune system produces autoantibodies that mistakenly target the skin, causing inflammation and the release of histamine. This results in redness, swelling, and intense itching. Additionally, autoimmune-related hives may be accompanied by other symptoms such as joint pain, fatigue, and swelling in different parts of the body.
Diagnosing Autoimmune-Related Hives
Diagnosing autoimmune-related hives requires a thorough evaluation by a healthcare professional. Blood tests may be conducted to check for autoantibodies, inflammation markers, and signs of an underlying autoimmune condition. In some cases, allergy testing and skin biopsies may be necessary to rule out other causes. Because chronic hives can sometimes be an early symptom of an autoimmune disorder, early diagnosis is crucial for effective treatment and management.

Treatment Options for Autoimmune Hives
The treatment of autoimmune-related hives focuses on controlling immune system overactivity and reducing inflammation. While antihistamines are commonly used to manage symptoms, more severe cases may require corticosteroids, immunosuppressants, or biologic drugs. Additionally, managing the underlying autoimmune disease is essential in preventing recurring outbreaks. Lifestyle modifications, such as stress management, dietary adjustments, and avoiding known triggers, can also help reduce flare-ups and improve overall well-being.
Living with Autoimmune-Related Hives
Living with chronic hives due to an autoimmune condition can be challenging, but with the right medical care and self-care strategies, individuals can effectively manage their symptoms. Regular monitoring of autoimmune conditions, working closely with a healthcare provider, and making necessary lifestyle adjustments can improve quality of life. Understanding the connection between hives and autoimmune disorders allows for better treatment approaches and empowers individuals to take proactive steps toward relief and long-term health.
Autoimmune conditions That Can Beget Hives
Several autoimmune conditions are associated with habitual hives. Below are some of the most common conditions linked to this skin response
1. Hashimoto’s Thyroiditis and Graves’ Disease
Both Hashimoto’s thyroiditis and Graves’ complaint are autoimmune diseases affecting the thyroid gland. Hashimoto’s leads to an underactive thyroid( hypothyroidism), while Graves’ complaint results in a hyperactive thyroid( hyperthyroidism).
Symptoms Fatigue, weight changes, mood disturbances, dry skin, and hair loss.

Connection to Hives Thyroid dysfunction can lead to vulnerable system imbalances that spark habitual hives. Some individualities with thyroid antibodies( similar to asanti-thyroglobulin or oranti-thyroid peroxidase) may develop hives as a vulnerable-mediated response.
2. Systemic Lupus Erythematosus( SLE)
Lupus is a habitual autoimmune complaint that causes inflammation throughout the body, affecting the skin, joints, and internal organs.
Symptoms common pain, fatigue, rashes, order issues, and photosensitivity.
Connection to Hives Lupus can beget acuity responses, where the vulnerable system attacks the skin, leading to urticaria. individualities with lupus frequently witness increased skin perceptivity, making them more prone to hives.
3. Dermatitis Herpetiformis( Associated with Celiac Disease)
Celiac complaint is an autoimmune complaint where gluten consumption triggers a vulnerable response that damages the small intestine. Some people with celiac complaints develop dermatitis herpetiformis( DH), a habitual skin condition characterized by itchy pocks and hives.
Symptoms Itchy, burning pocks on elbows, knees, and buttocks, along with digestive issues( if celiac complaint is present).
Connection to Hives DH is considered a form of autoimmune-affiliated skin inflammation, and avoiding gluten frequently reduces symptoms.
4. Rheumatoid Arthritis( RA)
Rheumatoid arthritis is an autoimmune complaint that primarily affects the joints but can also beget systemic symptoms, including skin issues.
Symptoms common pain, swelling, stiffness, fatigue, and fever.
Connection to Hives The habitual inflammation in RA can spark vulnerable responses leading to urticaria. also, some RA specifics may beget hives as a side effect.
5. Sjögren’s Pattern
Sjögren’s pattern is an autoimmune complaint that primarily affects humidity-producing glands, leading to dry eyes and mouth.
Symptoms Dry eyes, dry mouth, common pain, fatigue, and skin blankness.
Connection to Hives Due to vulnerable system dysfunction, individuals with Sjögren’s pattern may witness increased antipathetic responses, including habitual hives.
6. Vasculitis
Vasculitis is a group of autoimmune conditions that beget inflammation of the blood vessels, leading to reduced blood inflow to colorful organs and napkins.

Symptoms Skin rashes, fever, fatigue, muscle pain, and whim-whams damage.
Connection to Hives Urticarial vasculitis is a form of vasculitis that causes hives-like rashes. Unlike typical hives, these rashes last longer, are painful, and may leave bruising.
7. Autoimmune Urticaria
What Autoimmune Disease Causes Hives? Some individuals witness habitual hives due to direct autoimmune mechanisms without an associated systemic complaint. Autoimmune urticaria occurs when the vulnerable system produces autoantibodies that target the body’s mast cells, leading to histamine release and patient hives.
Symptoms habitual hives, angioedema( deep lump), and frequent flare-ups.
Connection to Hives The body’s vulnerable response inaptly attacks skin cells, resulting in long-term hives and swelling.
Diagnosing Autoimmune- Autoimmune-related hives
To determine if an autoimmune complaint is causing habitual hives, healthcare providers may perform
What Autoimmune Disease Causes Hives? Blood Tests To describe autoimmune labels( e.g., Corpus for lupus, thyroid antibodies for thyroid diseases, gluten antibodies for celiac complaint).
Skin Vivisection If vasculitis is suspected.
Elimination Diets To rule out food triggers.
Thyroid Function Tests To assess Hashimoto’s thyroiditis or Graves’ complaint.
Treatment Options for Autoimmune Hives
Managing hives caused by autoimmune conditions requires treating the beginning condition while addressing skin symptoms. Treatment options include
1. Antihistamines
First-line treatment for hives to block histamine release.
exemplifications Cetirizine, loratadine, fexofenadine.
2. Corticosteroids
Used for severe cases to reduce inflammation.
Long-term use is avoided due to side goods.
3. Immunosuppressants
specified for autoimmune conditions with severely vulnerable system overactivity.
exemplifications Methotrexate, cyclosporine.

4. Biologic curatives
Omalizumab( Xolair) is an injectable drug targeting IgE antibodies, generally used for habitual autoimmune urticaria.
5. Salutary and life Changes
barring gluten( for celiac-related hives), reducing stress, and avoiding given allergens can help control symptoms.
Maintaining a healthy diet with anti-inflammatory foods( e.g., omega-3s, fruits, vegetables) supports vulnerable balance.
6. Treating the Underpinning Autoimmune Condition
Controlling the autoimmune complaint with specifics and life variations can reduce or exclude hives over time.
Conclusion
What Autoimmune Disease Causes Hives? Hives can be a distressing symptom of autoimmune conditions, frequently persisting due to habitual vulnerable system dysfunction. Conditions similar to Hashimoto’s thyroiditis, lupus, rheumatoid arthritis, and vasculitis are common lawbreakers behind autoimmune urticaria. relating the underpinning cause is pivotal for effective operation and long-term relief.
Still, if you witness habitual hives, consulting a healthcare provider for proper opinion and treatment is essential. With the right approach, including drugs, life changes, and targeted remedies, individuals can manage autoimmune-affiliated hives and ameliorate their quality of life.
Read More: How to Dose Benadryl for Dogs: A Complete Guide
FAQs
Chronic urticaria (hives) is often linked to autoimmune conditions like lupus, Hashimoto’s thyroiditis, or dermatomyositis.
There is no definitive cure, but treatments like antihistamines, immunosuppressants, and lifestyle changes can help manage symptoms.
Autoimmune hives result from immune system dysfunction, while allergic hives are triggered by external allergens like food or pollen.
Triggers include stress, infections, hormonal changes, and underlying autoimmune conditions affecting the immune response.
A combination of antihistamines, corticosteroids, and immunomodulators helps reduce inflammation and control symptoms effectively.

